Glaucoma
Many people are familiar with the word “glaucoma” and they associate it with the eyes, but a large majority are unaware of the significance of the disease and how it can affect daily life. Glaucoma truly is a disease where the less you know about it, the more it can hurt you. It is one of the leading causes of blindness in the world according to the World Health Organization. In the United States, the most common form of glaucoma is open-angle glaucoma. This is a silent disease that slowly causes loss of peripheral vision and can eventually lead to blindness. It’s called “silent” because symptoms are almost always absent until the disease reaches an advanced stage. Sadly, once vision loss occurs from glaucoma, it’s irreversible.
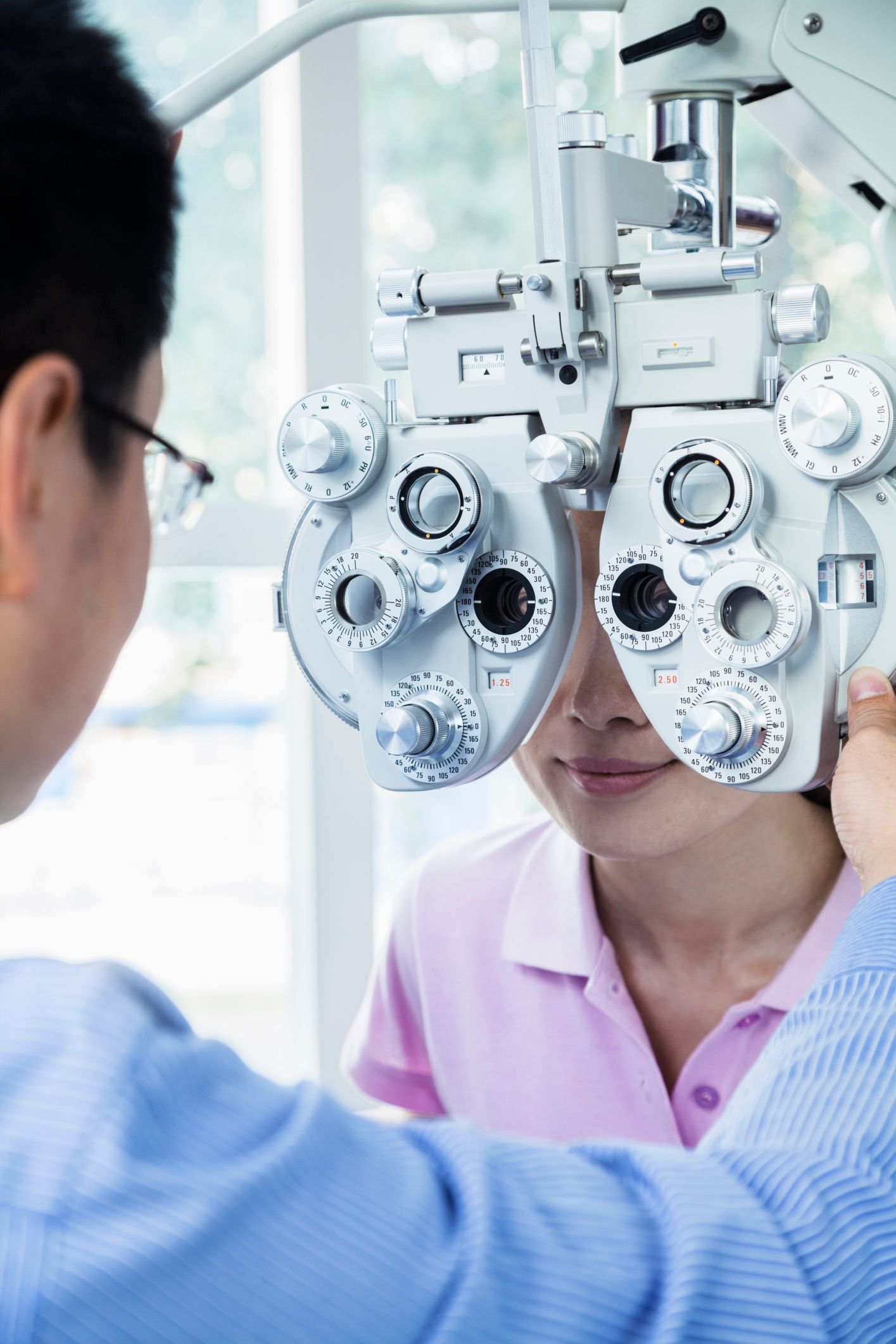
If a patient has risk of developing glaucoma, it’s critically important to be examined regularly by an eye doctor so that if glaucoma occurs, it can be treated. Glaucoma cannot be cured, but treatment can be very effective, especially when the disease is caught early. Keeping your eyes healthy through regular checkups is the best way to catch glaucoma early.
Treatment
Eye Doctors of Lancaster is blessed to have two expert, fellowship-trained glaucoma subspecialists, Dr. Justin Shaw and Dr. Shelley Mo, to help treat glaucoma in our community. Treatment for glaucoma presently consists of one primary goal—lowering eye pressure (intraocular pressure or IOP for short). IOP is determined by a balance between the volume of fluid made inside the eye vs the volume of fluid that leaves the eye over a given time. This fluid, called aqueous humor, is independent of the tear film that lubricates and protects the surface of the eye. Aqueous is made in the ciliary body which is located behind the iris, the colored part of the eye. It circulates through the pupil into the front segment of the eye called the anterior chamber, then drains out of the eye and into the veins of the eye socket (orbit) through an anatomic landmark called the angle of the eye.
Lowering IOP can be done by one of 3 methods: medication, laser and surgery. Because of increased risks, traditional glaucoma surgery is reserved for patients in whom glaucoma is worsening despite maximal medical treatment. Therefore, this discussion will focus on treatment using medications and/or laser. Although oral medications are available to treat glaucoma, bothersome side effects usually limit their use, so most glaucoma medications today are topical in the form of eye drops. These drops either reduce aqueous production, increase aqueous drainage or both. There are several different families of medicated eye drops, but just like medications for blood pressure control, each type of eye drop needs to be applied at least once daily and sometimes up to 3 times daily to keep the IOP controlled.
Laser Trabeculoplasty (SLT)
Instead of or in addition to medication, a laser treatment can be done to lower IOP. Although different types of lasers are used for various eye diseases, the type primarily used for open angle glaucoma is called laser trabeculoplasty. Last century, this was performed by an argon laser (ALT) that would burn tiny openings in the angle of the eye to allow aqueous to drain into the veins of the orbit more easily. Over the last few decades, however, an exciting advance has been made in laser technology called Selective Laser Trabeculoplasty (SLT). The laser energy (fluence) required for the SLT procedure is 4000 times less per laser pulse compared to ALT and lasts only 3 nanoseconds. This tiny amount of energy is absorbed by pigmented cells in the angle and causes no surrounding thermal damage. Instead, microscopic changes in the cells stimulate the body to remove debris from the angle. SLT essentially “tickles the immune system” in the eye and sends a message to clean out the angle and lower IOP “just like removing a clump of hair in a bathtub drain allows water to exit the tub more quickly”.
The laser effect usually reaches maximum IOP reduction after 8-12 weeks. One of the great things about SLT aside from its safety is that any IOP reduction that occurs persists for many months and even several years without the need for a patient to remember to use medicated eye drops every day. Once the IOP begins to rise months to years later, SLT can be repeated with good success. Eye Doctors of Lancaster is proud to have invested in this technology for the benefit of our glaucoma patients. SLT is performed in the office after numbing drops are applied, and the procedure takes only about 2-3 minutes to complete. While SLT is generally well-tolerated, some people might experience temporary discomfort or redness in the eye. If you have glaucoma and wish to see if this procedure may be for you or if you would like a thorough medical eye exam, please call to schedule an appointment at Eye Doctors of Lancaster.
Cataracts, Glaucoma and MIGS
It is not uncommon for patients to develop both cataracts and glaucoma, especially later in life. In addition to the use of medications and SLT to lower intraocular pressure as discussed above, patients can now consider Minimally Invasive Glaucoma Surgery (or MIGS) at the time of cataract surgery. Unlike traditional glaucoma surgery, the natural wall of the eye is not violated (except for the microscopic cataract surgery incision), so the long term risks of infection and hypotony (meaning the eye pressure dropping too low) is no higher than cataract surgery alone. Based on your unique circumstances and eye anatomy, your doctor may recommend one of several microstents (such as the iStent or Hydrus), Ab Interno Canaloplasty (ABiC), and/or Gonioscopy-Assisted Transluminal Trabeculotomy (GATT), all of which are various types of MIGS. Please watch the video below to learn more about MIGS.
Narrow Angle Glaucoma and Angle Closure Glaucoma
Laser Peripheral Iridotomy
Glaucoma Cyclo Diode Laser
Glaucoma Treatment Drainage Device
Trabeculectomy